Early-Stage Investigator (ESI) Committee
I obtained a PhD from the University of Kentucky in Toxicology. I then completed my postdoctoral fellowship at Vanderbilt University, where I studied how tumor cell glutamine metabolism suppresses anti-tumor immunity in triple-negative breast cancer. My current research interests focus on how metabolic interplay between tumor cells and the microenvironmental niche support metastasis to multiple sites, including bone and lung.
I’m a postdoctoral fellow in the lab of Dr. Jesus Delgado-Calle at the University of Arkansas for Medical Sciences in Little Rock, AR. I am interested in understanding the interactions between BCa cells and other bone cells in the metastatic niche. Using single-cell RNA sequencing, we found that osteocytes undergo profound cellular and molecular changes in BCa metastases. Being an expert in senescence, I quickly identified transcriptional changes indicative of premature cellular senescence and a senescence-associated secretory phenotype (SASP). We then carefully designed a series of experiments to determine if osteocytes undergo cellular senescence in BCa metastases and the functional consequences of this phenomenon. Using orthogonal approaches, I detected osteocytes with senescence-associated distension of satellites, telomere dysfunction, and p16Ink4a upregulation in form bones from mice and patients with BCa bone metastasis. Moreover, I demonstrated that clearance of senescent cells using senolytics decreases bone resorption and improves bone mass in mice with BCa bone metastasis. These findings highlight a previously unknown role of osteocyte senescence in initiating bone destruction in BCa metastases, offering new avenues for therapy.
I obtained my MS from Wake Forest University in 2021 Biomedical Science. I am now working towards my PhD where I study the FL/FLT3 axis in cancer-induced bone pain.
I went to the University of California, Merced, for my bachelor's degree in molecular and cellular biology. My project focuses on the role of Short-Form RON, an isoform of the receptor tyrosine kinase RON, in the anti-tumor immunity response against breast cancer bone metastasis. I specifically want to delineate the importance of specific immune cells in the anti-tumor response dependent on the loss of Short-Form RON.
My research focus as PhD (soon-to-be) candidate is the study of the Tubulin Code and its roles in both bone-metastatic breast cancer cells and normal bone development. Prior to my PhD I obtained a B.S. in Biochemistry at Loyola University Chicago and worked as a lab technician with a molecular biology focus.
I received my B.S. from the University of Indianapolis and my M.S. from Marian University. I am currently a fourth-year Ph.D. candidate at UAMS in the graduate program in biomedical sciences in the laboratory of Dr. Jesus Delgado-Calle, where I study bone-targeted therapies to treat multiple myeloma. My research focuses on the effects of Notch inhibition and Wnt activation on tumor, bone disease, and dormancy in multiple myeloma.
I obtained my PhD in Biomedical Engineering at Stony Brook University in NY and completed my post-doc at Indiana University. As Assistant Professor at MD Anderson Cancer Center, my research focuses on the cancer-induced bone disease and its response to its mechanical environment.
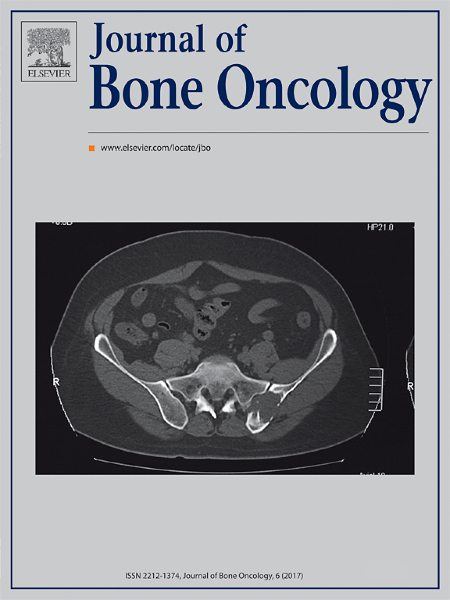
The effects of parathyroid hormone-related protein (PTHrP) on breast cancer bone metastasis patterns.
I obtained a PhD from the Technical University of Dresden (Germany) where I investigated how extracellular vesicles (EVs) derived from prostate cancer cells contribute to the formation of a pre-metastatic niche within the bone. Currently, my research interests focus on understanding the mechanism by which bone-derived stromal populations infiltrating extra-skeletal tumors modulate malignant cell behavior and immune responses.
I obtained a MS in Biomedical Science from Wake Forest University in 2022 where I studied the role of angiotensin II in cancer-induced bone pain. I am now pursuing my PhD in Dr. Yusuke Shiozawa's lab where I focus on understanding the crosstalk between the gut microbiome and prostate cancer bone metastasis.
I received my PhD from the University of Sheffield, UK studying how the NFkappaB pathway affects breast cancer bone metastasis. I then moved to the United States to pursue a postdoctoral fellowship in multiple myeloma in the lab of Conor Lynch. During this time, I identified novel mechanisms of drug resistance. My current research focus is understanding how age alters multiple myeloma progression and bone disease.
I am currently a postdoc at Mayo Clinic examining the role of therapy-induced senescence in ERa+ breast cancer progression with a hope to merge my previous training on bone osteoimmunology to pursue an independent research in breat cancer bone metastasis.
I’m a 4th-year Ph.D. candidate at Rush University Medical Center in Chicago, IL. My interest in bone metastasis was sparked by the limited treatment options and the need for a multidisciplinary approach. My lab focuses on understanding cytoskeletal changes in bone metastatic breast cancer cells. My project aims to establish a correlation between the differential expression of tubulin isotypes and overall survival in bone metastatic breast cancers. My goal is to identify the tubulin code and its regulators, seeking novel microtubule-targeting strategies to hinder the bone metastatic potential of breast cancer cells. This research has the potential to pave the way for personalized chemotherapy regimens and improve patient care.
I received my BS in Biotechnology from the University of California, Davis in 2014 and then spent 6 years working in industry, including a position in Biologics Manufacturing at Genentech and positions in Molecular Biology and Immuno-oncology at Five Prime Therapeutics, where I worked on screening and mechanistic studies for novel immune checkpoint inhibitors. I matriculated into the University of Michigan's Cancer Biology gradaute program in 2020 and joined the lab of Dr. Megan Weivoda. Since then, I have become a PhD candidate and moved with the Weivoda Lab to the Mayo Clinic in Rochester, MN to complete my dissertation work. I focus on the role of therapy-induced senescence and myeloid-like plasticity in multiple myeloma dormancy and relapse. Multiple myeloma is an incurable plasma cell cancer with heavy involvement in bone, and I have put my efforts towards elucidating how chemotherapies commonly used in the standard treatment of the disease can drive the formation of senescent-like tumor cells with a distinct myeloid signature. Furthermore, I am exploring how this myeloid-like lineage plasticity can drive osteoclast-like behaviors in multiple myeloma cells and influence osteoclastogenesis within the bone marrow microenvironment. We are ultimately interested in correlating these phenotypes with patient outcomes and providing evidence for new targets to ablate relapse post-therapy.
I am a current graduate student in the laboratory of Dr. Roberta Faccio at Washington University in St. Louis. My researched is focused on understanding how primary breast cancer affects hematopoietic stem and progenitor cells (HSCPS) in the bone marrow to drive systemic alterations in the immune landscape and immunosuppression.
I graduated from the University of Iowa with a B.S. in biochemistry, where I wrote my undergraduate thesis on the development of small-molecule inhibitors for a DNA repair protein known as RAD52. Now, I am in my 3rd year at Vanderbilt University and as a Ph.D. candidate in the lab of Dr. Julie Rhoades I have developed a strong interest in the ways in which the bone microenvironment enables heightened resistance to chemotherapy. Specifically, my dissertation research is concerning the role of Hedgehog and Transforming Growth Factor beta in the acquisition of resistance to chemotherapy in skeletal metastases of triple-negative breast cancer. My goal is to clarify the molecular mechanisms by which Hh/TGFb crosstalk results in upregulation of efflux transporters and ultimately, recurrence of tumors. I look forward to applying my experiences in basic sciences research towards the development of bone-targeted therapies for patients with treatment-resistant cancer. Beyond my Ph.D. my career goal is to contribute towards the development of cancer therapeutics through research in the setting of academic drug discovery.
I received my MS in Biomedical Science from Wake Forest University in 2023 studying fibroblasts and their association with prostate cancer-induced bone pain. I am currently a graduate student in Dr. Yusuke Shiozawa's lab where I now study colorectal cancer chemotherapy-induced peripheral neuropathy and cancer-induced bone pain.